SUNDAY, 7 NOVEMBER 2010
Wendy Mak, Maja Choma and Jack Green take you on a journey through the past, present and future of gene therapy, the hurdles this technology has faced and why it is becoming accepted in mainstream medicine.The Beginnings of an Idea
The concept that DNA can be shuffled between cells to change their behaviour is extraordinary, but this feat is achieved naturally by the simplest of organisms and can be easily replicated within modern molecular biology laboratories. A revolution in the understanding and manipulation of DNA has led the way into a new world of scientific and medical capabilities, with gene therapy at the cutting edge. Yet the humble origins of this technology lie with a cautious British medical officer and a troublesome little bacterium.
In the 1920s, Frederick Griffith was working on classifying strains of Streptococcus pneumoniae, the bacterium responsible for pneumonia, when he made a startling discovery. He found that when a normally harmless strain of the bacterium was injected into a mouse along with dead cells of a pathogenic strain, the mouse became ill and died. This suggested that the harmless strain could transform into the pathogenic one when simply accompanied by dead cells that had been pathogenic. Researchers later realised that the non-virulent form of Streptococcus received and integrated a segment of DNA from the pathogenic form. The DNA was physically transferred from one cell to another and contained information that led to the transformation. Little did Griffith realise that his discovery was to begin a journey into the understanding of the genetic code.
Following this breakthrough in bacteria, work quickly moved on to transforming mammalian cells using DNA transfer. Szybalska and Szybalski demonstrated in 1962 that human cells lacking an enzyme that breaks down uric acid were able to take up DNA from wild-type cells and subsequently produce the functional enzyme. With this experiment, the conceptual groundwork of gene therapy was laid: functional versions of genes could be used to replace defective versions in mutant cells.
The early methods of cell-to-cell gene transfer were inefficient, but in the 1970s new techniques led to dramatic improvements. Newly discovered enzymes allowed sections of DNA to be cut from chromosomes with incredible precision and stuck into other segments of DNA from completely different organisms; the result was a recombinant DNA molecule. With this technology in place, scientists began to contemplate using gene therapy on people.
The earliest applications of gene therapy in humans proved to be a bitterly contentious affair. It was 1980 when an American lab led by Martin Cline made the first, ill-fated attempt at human gene therapy using recombinant DNA. Cline was a rare breed of scientist who combined clinical practice with an expert knowledge of cutting-edge molecular biology. The first isolation of a human gene, called beta-globin, had been achieved, and with an eye on the brimming therapeutic potential of gene therapy, Cline was in a hurry to put this knowledge to good use.
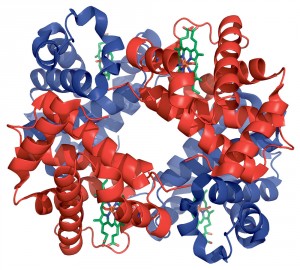
Cline wanted to use gene therapy to treat beta-thalassaemia, a genetic blood disorder characterised by reduced production of haemoglobin (the oxygen-carrying molecule of the blood). People with the disorder often suffer from anaemia, fatigue and other more serious symptoms. It is caused by a mutation in beta-globin, which is one of the two protein chains that make up haemoglobin. Cline’s lab established that the human beta-globin gene could be introduced into mouse bone marrow cells in vitro, and that these genetically modified cells could repopulate niches cleared by irradiation in the marrow of a recipient mouse. With the same experimental framework, he set out to repeat this work in human patients with beta-thalassaemia. Would it be possible to remove these patients’ bone marrow cells, replace their defective globin gene with a functional copy, and reintroduce the corrected cells to cure their disorder?
Unfortunately it was not to be; not only were the results inconclusive, but the experiment sparked much public criticism and anger. Cline obtained permission from ethical committees to inject into patient cells the naked form of the human globin gene, but not the gene tacked onto the bacterial scaffold. Cline argued that the bacterial section of DNA contained another important gene that would give the treated cells a growth advantage over uncorrected cells and make success more likely. Despite the lack of permission, Cline went ahead and injected both human and bacterial DNA into the patients’ cells. This left many with doubts over whether scientists could be trusted to behave responsibly with these new and potentially dangerous technologies. In the end, Cline lost his funding and resigned from his university position.
Although it was a controversial start, enthusiasm for gene therapy was not dampened. A consensus emerged that, had Cline waited for more animal research to confirm the safety of the recombinant DNA, he would have undoubtedly obtained ethical approval; it was his haste that was his downfall. Gradually, a body of interest grew into a more confident field. Now, a new chapter of gene therapy has begun. The first successes in humans have been reported and new treatments are starting to become medical realities.
Gene Therapy: Success and Triumphs
The field of gene therapy is still developing, and most diseases cannot be treated with current technology; however, there have been some significant successes, where gene therapy has cured or helped to treat some devastating conditions.
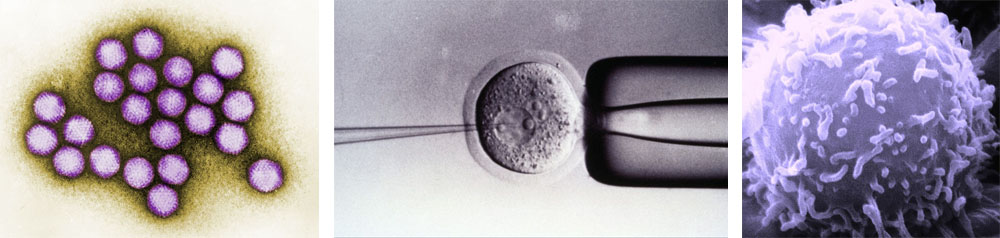
Imagine living your life without an immune system: you would be prey to any pathogen that comes your way. A common cold could kill you. This is what patients with severe combined immunodeficiency disorder (SCID) have to deal with. They have a faulty gene that prevents their bodies from producing T lymphocytes, a major component of the immune system. This means that their immune system is incredibly weak and many patients must deal with major infections from early on in their lives.
Until recently, the only effective treatment was a bone marrow transplant. However, this is not an ideal remedy, as a matching donor must be found, and the transplant can be rejected. Gene therapy provides a more elegant solution; simply correcting the problem gene allows the body to produce T lymphocytes normally. Unfortunately, the first clinical trials using gene therapy to treat SCID ran into major problems, as the treatment triggered cancer in some patients. Nonetheless, a recently completed 10-year trial proved to be much more successful, allowing several patients with SCID to live essentially normal lives. While there are certain side effects, all of the patients are still alive, and none of them have had problems with cancer.
Leber’s congenital amaurosis (LCA) is an inherited eye disorder in which patients suffer from vision deterioration and eventual blindness. Since the condition results from a single abnormal gene, it is an ideal candidate for gene therapy, especially considering there are no other treatments available.
In 2008, researchers at UCL and Moorfields Eye Hospital in London completed a clinical trial of a novel gene therapy treatment for LCA. The correct version of the gene was injected directly into the retinal cells of patients. Tests after the treatment showed no evidence of side effects, and one patient gained significant improvement in his night vision.
As the trial was conducted on adult patients whose disease progression was already highly advanced, this likely masks the true potential of the treatment. Trials have now begun on younger patients who will hopefully benefit significantly more.
Cystic fibrosis is one of the most common life-threatening inherited diseases, especially among people of European descent. Sufferers have no working copy of the CFTR gene, which produces a protein that regulates the salt balance in the body. As a result, internal organs become clogged with a thick mucus, making sufferers prone to infection, especially in the lungs, and causing other problems such as difficulty in digesting food. The hope is that gene therapy could be used to insert a functional copy of the CFTR gene and thus allow patients to live normal lives.
Advances in medical knowledge have increased the life expectancy of cystic fibrosis patients, but it is still short (approximately 48 years) and at present there is no cure. Although all cells of the body are affected, it is incredibly challenging to insert a new gene into every cell. Thus, current efforts are concentrated on inserting the gene specifically into the cells of the lungs, as some of the most debilitating symptoms of cystic fibrosis affect this organ.
A pilot study involving 16 patients was completed in 2009. The therapy was found to have no major side effects and several patients produced levels of working protein comparable to healthy people. Due to the fact that treated cells die after a certain period of time, repeated treatments are almost certainly necessary. A full scale trial is now underway with a multi-dose treatment regime.
Cancer is a complex disease resulting from many genetic alterations acquired over many years. However, gene therapy does offer a feasible treatment. Cancer cells can be targeted directly by introducing genes that drive them to commit suicide or slow their replication. A current study is using this approach in patients with advanced lung cancer.
Patients’ immune cells can also be modified to make them attack cancer cells, an approach that has already been used to treat melanoma, an aggressive form of skin cancer. Lymphocytes were removed from the patient and new genes were inserted into them. Upon reintroduction to the body, the lymphocytes were able to identify cancer cells and attack them. In a study completed in 2006, 17 patients with advanced melanoma were treated using this method; most of their cancers were reduced and there were no significant side effects reported.
The most exciting aspect of this area of research is that the techniques used in these studies should be applicable to a wide range of cancers, offering the hope of a universal cure for cancer.
Gene Therapy in Practice
Delivery of a gene, although relatively straightforward in cultured cells, presents many problems in the context of patients. The safety of a strategy is always the principle concern, but there are also many other considerations. How do you deliver the gene into the cells? How do you get the gene into the right cells? How do you get enough of the cells to express the gene? All of these questions present considerable technical challenges.
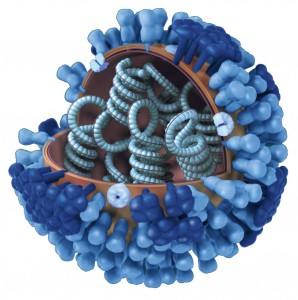
The ideal approach for gene therapy would be to remove the cells of interest and transfect them with the new gene outside of the patient’s body. This would allow specific cell types to be easily targeted, and treated cells could be screened for unintended or dangerous changes before reintroducing them into the patient. Unfortunately, this is only possible with a few tissue types, such as blood and skin. Often it is impossible, for example with the brain and heart, and gene therapy must be applied inside the patient. This requires a vector that can carry DNA past the immune system, reach the target cells, and overcome intracellular mechanisms that protect against foreign DNA. To find a suitable vector, the field of gene therapy has turned to viruses, which make their ‘living’ by efficiently introducing large amounts of DNA into cells. Using viruses, however, is not without risk.
There are many viral candidates to choose from, and many factors must be considered when selecting one. Firstly, the virus must target the correct cells for the genetic disease to be treated. For example, some diseases require a virus that affects only dividing cells, whereas in others it must target a particular tissue. However, no single candidate meets all of the criteria for a safe, efficient and effective vector, so the choice must be made carefully.
Most importantly, a potential viral vector must be well-known and thoroughly studied. It is therefore no surprise that many viruses used in gene therapy are closely related to pathogenic viruses. For example, adenoviruses, which cause the common cold, can also be used in gene therapy to target cells within the lungs and respiratory tract. The herpes simplex virus, which causes cold sores, can be used to target cells in the brain. And retroviruses, which include HIV, are useful because they are incredibly good at avoiding the immune system. But because these viruses are related to those that cause disease, there are dangers. An ideal vector would be completely safe and unable to revert to its virulent form, but it is impossible to eliminate all risk.
To ensure that a vector is as safe as possible, the virus is engineered to prevent replication and screened for its ability to cause cancer and elicit an immune response. Despite these precautions, vectors can still cause serious harm. Adenoviruses have been used for gene therapy but they can also elicit strong immune responses; in one trial, the immune response induced by the adenovirus actually killed a patient. Retroviruses insert their DNA directly into the patient’s DNA and therefore there is a risk that this will disrupt a vital gene or activate a cancer-causing oncogene. This was the case for some patients in the first human gene therapy trial to treat SCID. One quarter of the patients developed leukaemia, which was fatal in two instances.
Safety is of paramount importance, but it must also be balanced with the efficiency of treatment. This is particularly relevant in the case of retroviruses. While the insertion of a new gene into the patient’s DNA runs the risk of disrupting normal genes or causing cancer, it usually results in higher expression and more efficient transmission during cell replication, which ensures that the gene is retained over time. The risks can also be reduced; a recently developed HIV-derived virus inserts its DNA randomly throughout the genome, decreasing the chance that an important gene will be disrupted in a significant number of cells. A virus that does not integrate, such as an adenovirus, carries less risk but requires repeated treatment and may not be as effective.
There are further difficulties in choosing a viral vector, caused by the large size of mammalian genes. A vector must be able to carry large amounts of DNA, but most viruses are small and struggle to hold the genetic information that codes for most proteins. Herpes simplex virus can transport almost 20 times as much DNA as other viruses but still cannot carry the dystrophin gene, admittedly the largest known mammalian gene, but also one that is targeted in the treatment of muscular dystrophy.
Our limited understanding of what causes many diseases also limits the application of gene therapy. When there is a defect in a single gene that codes for a protein with a known function, it is relatively easy to design a remedy using gene therapy. However, for more complex diseases such as cancers or neurological conditions, it is unclear which genes to target because we don’t fully understand how these diseases work. We are also helpless when faced with disorders where the damage occurs early on in development, such as Down’s syndrome. Furthermore, we are at a loss for how to target common conditions such as obesity or high blood pressure, because the genes identified so far are linked to only small increases in risk.
Gene therapy is still far from a perfect treatment and it is often only used as a last resort for the most serious diseases, where the risks associated with treatment become acceptable. Many challenges still remain and if we are to make the technology safer and more widely applicable, we not only need better tools for gene delivery but also a more complete understanding of the diseases we wish to treat. Gene therapy has come a long way since its early days and it is finally delivering some real treatments for serious diseases. The success of recent trials highlights the promise of this amazing technology.
Wendy Mak is a PhD student in the Department of Physics
Maja Choma is a PhD student at the Cambridge Institute for Medical Research
Jack Green is a PhD student in the Department of Zoology