MONDAY, 3 FEBRUARY 2014
Imagine having sandpaper between your joints, scraping painfully with every movement. This is the experience of many of those living with alkaptonuria, a rare genetic disease affecting nearly 1000 people worldwide. Alkaptonuria involves the disruption of a metabolic pathway for degrading two amino acids, phenylalanine and tyrosine. As a result, homogentisic acid (HGA), an intermediate, builds up and circulates in the blood at high levels. Unlike the build- up of intermediates in many other metabolic diseases, HGA is not actually immediately harmful. It is highly water-soluble and thus easily removed via urine. Alkaptonuria patients can excrete grams of HGA daily. It is the HGA in urine that gives rise to the main symptom of the disease. On contact with air, HGA oxidises and turns the urine black. The diagnosis of alkaptonuria in newborns is often brought about by the sight of black urine in nappies.As alkaptonuria patients age, the circulating HGA accumulates in structural tissues, particularly affecting collagenous tissues such as joint cartilage. Through a process known as ochronosis, which is still not well understood, the accumulated HGA oxidises into a dark brown pigment that cannot be removed. HGA also accumulates in heart valves, spinal discs, trachea, and the kidneys, which visibly darken. Dark spots are sometimes observed in the whites of the eyes and ear cartilage.
As well as pigmenting tissue, ochronosis prevents natural turnover and repair processes, and leads to mechanical changes in cartilage, making it hard and brittle. Ochronotic cartilage fails to provide shock absorbance and usually leads to abrasive action with any joint movement. By the time they reach their thirties, many patients suffer from symptoms similar to osteoarthritis as a result of the deterioration of their joints, and will often require their first joint replacement before they turn forty. Many alkaptonuria patients will eventually require multiple joint replacements and experience significantly reduced mobility and pain in their daily lives. Ochronosis, once it has set in, also leads to cardiovascular problems and recurring kidney stones, with little that can be done to restore the tissues. The main hope for a cure for alkaptonuria is to reduce HGA production before the onset of ochronosis.
In the course of searching for a treatment, the genetic and biochemical basis of alkaptonuria has been investigated. While there are only 64 diagnosed alkaptonuria patients in the UK, the incidence of alkaptonuria varies from an average of 1 in 250,000 to higher in particular ‘hotspots’ found in countries such as Jordan, India, the Dominican Republic, and Slovakia (for which the incidence is 1 in 19,000). Some of these hotspots are believed to be linked to the cultural practice of consanguineous marriage, that is, marriage between relatives, such as first cousins. Alkaptonuria is a recessive disorder; the mutation may spontaneously arise in a person, the ‘carrier’, such that they have one functional and one defective gene, but appear healthy otherwise. Consanguinity between the offspring of a carrier increases the chance that future offspring will have two copies of the defective gene and thus have the disease. The enzyme that is affected in alkaptonuria is hexametric, hence there are many genetic mutations that could disrupt the assembly of the functional enzyme and lead to the disease.
Alkaptonuria was first reported by Sir Archibald Garrod in 1899. Now, more than 100 years later, there is still no treatment. One alkaptonuria patient, who also has hepatitis B, was found to stop producing HGA in his urine after receiving a liver transplant. However, as alkaptonuria is not an immediately life-threatening disease, it is difficult to justify giving a transplant to an alkaptonuria patient who is otherwise healthy in preference to other patients with more severe liver failure. In principle, a full liver is not required as a single lobe can grow back to full size. However, taking even part of a liver from a live donor is fraught with complications, and the receiver will have to take anti-rejection drugs for an extended period, possibly for their whole life, making this treatment route unfavourable.
Another method to reduce HGA would be to use enzyme or genetic therapy to deliver an enzyme, or gene that can produce the functional enzyme, into liver cells of alkaptonuria patients. Thus, HGA could be processed as intended, and eventually reduced to a normal level. While promising in principle, the mechanism for delivery of enzymatic or genetic material is still being developed, with no clinical candidates yet. Moreover, even in the most optimistic timescale from initial development to clinical use, it would be 5–10 years before these treatments reach alkaptonuria patients.
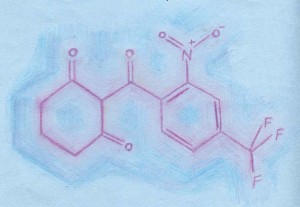
The most promising treatment to date is the drug nitisinone, which was first developed as a weed killer and then found to be useful for treating hereditary tyrosinemia type 1, a severe metabolic disorder that is fatal in childhood if left untreated. Nitisinone inhibits the enzyme that produces HGA in the defective metabolic pathway. Taking nitisinone daily can return blood HGA levels to normal. As nitisinone is already used in treating tyrosinemia, it is known to be relatively non-toxic. However, using nitisinone to treat alkaptonuria is not yet an approved procedure, and does have side effects: it increases the blood tyrosine level, which can lead to blurring of vision, skin rashes, and potential cognitive effects, especially in children whose brains are still developing. Thus, nitisinone is usually administered in conjunction with a low protein diet in order to minimise these adverse effects.
As the long-term safety of nitisinone is still unclear, further clinical trials are necessary before it can be approved as a treatment for alkaptonuria. While NHS patients can receive the drug off- label, the limited number of patients and funding meant that a UK trial was not carried out. In addition, placebo controlled trials are not possible as patients can easily find out if their urine has stopped turning black.
The Cambridge-based patient group Alkaptonuria Society has recently secured funding to launch two nitisinone trials, and ran a successful Indiegogo crowdfunding campaign, raising 121,000 USD to assist patients in accessing these trials. The society is also highly active in raising awareness, educating patients, and collaborating with scientists and clinicians. In October 2013, the seventh international scientific workshop on alkaptonuria was held in Liverpool, showcasing a diverse range of research into understanding and tackling the molecular basis and pathologies of this disease.
Although not all rare disease sufferers have such good links with scientists and funding bodies, the Alkaptonuria Society is leading by example, inspiring the development of a new charity called Findacure. This aims to act as an umbrella organisation to help other rare disease sufferers form strong patient groups. In addition to improving the lives’ of sufferers, the study of rare diseases can help us understand processes that are fundamental to health. Indeed, Alkaptonuria has already provided insight into the more common process of osteoarthritis. Sir Archibald Garrod, the early 20th century physician first to postulate a cause of black bone disease, wrote, “The study of nature’s experiments is of special value; and many lessons which rare maladies can teach could hardly be learned in other ways.” The Alkaptonuria Society provides a precedent upon which future efforts to understand and tackle “nature’s experiments” can be built; the outcomes may well benefit all of us.
WingYing Chow is a postdoctoral researcher in the Department of Chemistry