FRIDAY, 20 MARCH 2020
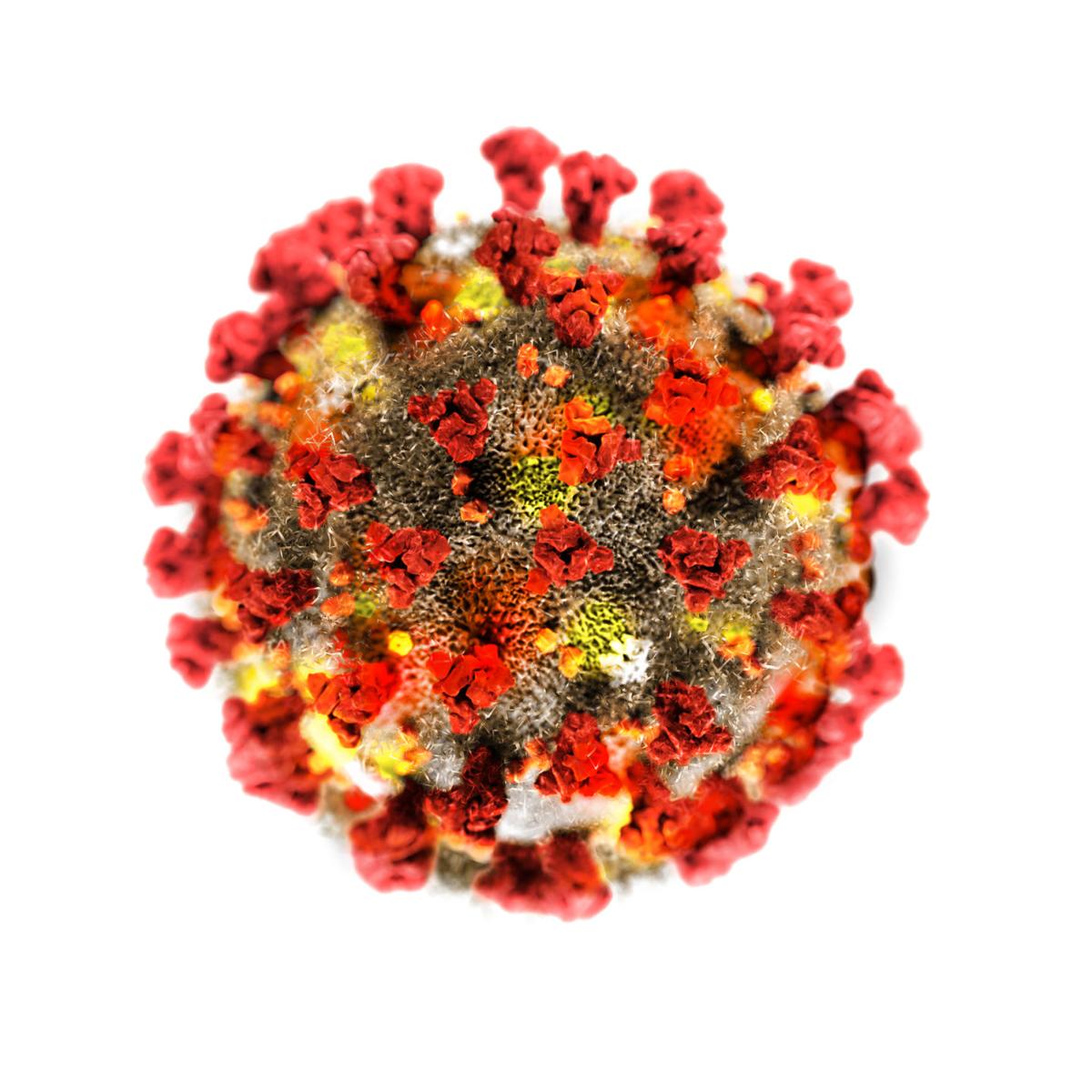
Coronaviruses represent a diverse family of enveloped RNA viruses that infect mammals and birds, and are so named because they feature a prominent spike protein on their outer surface, resembling a crown (Latin: corona). They are notable due to their evolutionary flexibility resulting from their high mutation rate. In fact, coronaviruses accumulate a single mutation every 4 days on average[1], which is impressive given that the viral genome itself is only ~30,000 base pairs in length, corresponding to a 0.3% chance of a mutation at each point in the genome each year. As a result, a coronavirus strain endemic to a given species can rapidly mutate to infect new naïve species by varying the structure of its spike protein and thus its ability to infect different types of cells. Due to this, each crossover event is typically associated with great socioeconomic cost, whether through the loss of large quantities of economically important livestock, or by causing severe disease and death in a large fraction of the human population. These outbreaks are difficult to predict due to the sheer diversity and quantity of coronavirus genomes and the speed at which they mutate.With the latest outbreak, a coronavirus strain that primarily infected bats seems to have undergone key mutations in an unidentified intermediate species that allowed it to cross over to humans at some point in November 2019[2]. The virus then began circulating in a bush meat market in Wuhan during December 2019, where it infected the majority of stall owners and customers. It was rapidly recognised as being similar to the pathogen responsible for severe acute respiratory syndrome (SARS), despite being less fatal, however the implications of this finding were initially overlooked by local health authorities[3]. Due to this, the virus was able to spread rapidly across China and further afield via the city's extensive road, rail and air networks. By the time the infectivity of the virus was acknowledged, the virus had already established itself in eastern China, and internationally countries were beginning to report index cases. It was also at this time that the virus was named SARS-CoV-2 in light of its genetic similarities to the SARS coronavirus, and the name of the disease that it caused was renamed COVID-19.
In spite of an unprecedented effort by the Chinese government to shut down entire cities in an attempt to contain the spread of the virus, international containment efforts failed due to the near simultaneous occurrence of outbreaks in Italy, South Korea, and Iran. This set the stage for a global spread of the virus due to the initial reluctance of countries to close off borders and initiate large scale quarantines and testing. While these measures were ultimately adopted in a patchwork fashion, this was not enough to stop the current explosion of outbreaks now seen across North America, Eurasia and Oceania.
What is it?
The defining feature of this clade of coronavirus (Sarbecoviridae) is that it primarily enters cells by binding to angiotensin converting enzyme (ACE2). This is a surface bound enzyme involved in the regulation of blood pressure. It is found throughout the body, particularly on the internal lining of all blood vessels and in the cells of the immune system, heart, kidneys and lungs.
The course of infection by SARS-CoV-2 features a transient immunosuppression in which the virus infects and destroys the immune cells normally needed to detect and destroy virus-infected cells[4]. At the same time, it rapidly infects and replicates within lung tissue. In the process, the capillaries in the lungs begin to bleed, producing well-defined, hazy patches on a CT scan characteristic of atypical pneumonia. While most people will present to hospital at this point with a fever and cough, up to 20-50% may initially experience no or minimal symptoms when they first test positive[5], as it can take up to 12 days for symptoms to develop[6]. In light of the extensive distribution of ACE2 in the body, the virus has also been known to infect the gut, kidney and brain, causing diarrhoea, vomiting, acute renal failure and encephalitis respectively[7].
In most people, this immunosuppression resolves over the next few weeks as the symptoms resolve[8], although it appears that some limited viral reproduction, possibly in the lower airways, can still take place for up to 2 weeks following the cessation of symptoms. Following recovery, there is evidence that antibodies against SARS-CoV-2 are retained after the initial infection[9]. Even so, anecdotal cases of reinfection have been reported. It is unclear whether this is because the natural immunity disappears after a period of time, as is the case with SARS, or whether the high mutation rate of the virus allows it to generate strains that can evade this immunity, or even if the reported cases were due to false negative test errors.
In a significant minority of infected people, this immunosuppression then persists[8], in which case unchecked viral reproduction causes lung tissue to die off faster than it can be broken down, in a process known as coagulative necrosis. The resulting debris and fluid can then plug the airways, leading to respiratory failure. Furthermore, the immune system can become overactive as the infection is eventually cleared, producing further organ damage, among other things.
Is it treatable?
There are a few opportunities to exploit existing drugs to treat coronavirus infections. Surprisingly enough, the use of antimalarial drugs such as chloroquine and its derivatives have been recommended by Chinese, South Korean, Dutch and Polish guidelines on the basis of evidence that it can shorten the course and severity of infection. These drugs work by interfering with the process of cellular engulfment of the virus, slowing down the speed at which the coronavirus can infect cells, while also reducing the extent of the inflammatory response to dead lung tissue. They may also help to increase the concentration of zinc in cells, which may serve to inhibit viral replication.
More conventionally, antiviral drugs originally designed for use against RNA viruses such as hepatitis C and HIV may be used to interfere with viral replication in the host cells. These include the nucleoside/nucleotide analogues ribavirin, umifenovir and remdesivir as well as the protease inhibitors lopinavir and ritonavir. Inhaled low dose steroids and interferon can also be used with care to control the intensity of the immune response in the lung.
Infusions of neutralising antibodies can also be used to slow the spread of the virus between cells. While this can be achieved by extracting antibodies from the serum of recovered patients, supplies of these are limited. However, a San Francisco-based company[10] and a Dutch team of researchers[11] have both been able to create monoclonal antibodies against the coronavirus, which will reduce the reliance on serum from recovered patients to provide neutralising antibodies once production can be scaled up.
That said, the bulk of the treatment is still largely symptomatic in nature, and is centered around supplementing or augmenting lung function. Thus, standard treatment might involve providing patients with oxygen while placing them at a 30 degree incline and performing regular lung suction to reduce the risk of choking on their lung secretions. More invasive options such as ventilation, low viscosity air mixes or extracorporeal membrane oxygenation are then reserved for more severe cases.
Why should we be worried?
It is important to realise that the novel coronavirus is more of a public health issue than a direct threat to life to those without preexisting medical conditions. The available data suggests that the percentage of people who die from SARS-CoV-2 is just under 1% on average, but when the healthcare system is overwhelmed, as is the case in Wuhan, Italy or Iran, the mortality rate is closer to 3-5%. The rate is also strongly dependent on age, roughly doubling for every 10 years of age above age 50, peaking at about 15% for people over 80 years of age. Thus, countries with an aging population will be disproportionately affected[12].
It is important to realise that the novel coronavirus is more of a public health issue than a direct threat to life to those without preexisting medical conditions.
The main issue is epidemiological. If left unchecked, each patient will infect, on average, 3 other people over the course of their illness, resulting in a doubling in the number of infected people every 2.5 days or so. At least a fifth of sufferers, regardless of age, will require medical help for their symptoms, of which some proportion will require intensive care[13]. This creates an issue once the number of infected patients exceeds the number of available hospital beds.
For reference, the OECD average for hospital bed numbers stands at 5 beds per 1000 people, with the UK being at just over half of this figure. On average, three quarters of hospital beds are in use at any given time, but this number can be readily changed by rescheduling operations or rationing healthcare. Thus, if COVID-19 was allowed to infect even 10% of the population, hospital bed availability would need to increase fourfold or more over a short span of time, with the required number of beds quadrupling every week or so.
Even if the necessary additional bed space could somehow be built in time, the entire healthcare system will become strained as healthcare professionals fall ill and as supply chains struggle to rapidly ramp up production of key items such as medicines, face masks or ventilators, due to the long lead times required and the lack of inventory. Overall mortality will go up as all patients, not just COVID-19 sufferers, are unable to receive the healthcare they need.
How can governments stop it?
In order to avoid the chaos that would result from a breakdown of a country's healthcare system, countries must take action from an early stage to halt the spread of the virus and eradicate it. It is a fallacy that warmer weather and high humidity alone will stop the disease, both because outbreaks are already taking place in tropical countries, and because the seasonality seen in the flu virus is only possible due to the presence of herd immunity within the population[14]. Moreover, herd immunity relies on the assumption that the immunity from an infection will last a lifetime, which was not the case with SARS[15]. This opens up the possibility that the global population will continue to be ravaged by economically devastating outbreaks of this virus in the near future, unless an effective vaccine can be developed.
Instead, countries must effect extensive changes in social behaviour. Large gatherings of people are hotbeds of infection as everyone there is at constant risk of being coughed or sneezed upon, or of infecting themselves by touching a contaminated surface. Ultimately, hundreds if not thousands of people can be infected over a short period of time, defeating any attempts at containment. Thus, action must be taken to not just cancel headline grabbing events such as tours, concerts or religious gatherings, but also things that we take for granted such as restaurants, public transport or schools.
At the same time, countries must actively look for index cases - infected individuals who cannot be attributed to an existing cluster of infections. This involves screening for symptoms such as fever or cough at high risk locations like ports of entry, schools or hospitals, and then quarantining and/or testing those who fail. They must then take proactive action to actively track down and test anyone who might have been in contact with any infected individuals, as well as their contacts. This increases the likelihood that any infected individuals will be detected and isolated regardless of the severity of their symptoms, reducing the number of people they can spread the disease to. However, this alone will not stop community spread. This is because the latent period, during which the patient is infective but asymptomatic, typically lasts for ~5 days but can last for up to 10 days or more[16]. In fact, most onward transmission occurs in the first few days during this asymptomatic, latent period. The average interval between cases in a transmission chain is also ~5 days[17], indicating that on average, this is around the point where onward infection of others is most likely to occur.
Even so, about 80% of infected people, particularly younger people, will experience mild symptoms indistinguishable from the flu, and might thus be overlooked. If this happens sufficiently frequently, transmission within a minimally symptomatic pool of infected people in the community can, and will, become self sustaining. In this situation, mass testing of patients with influenza-like symptoms and, in later stages, of the whole population is the only option. Even though this may result in high levels of false positives, this is necessary to maintain population morale by providing full insight into the spread of disease, while also justifying the need for future targeted population quarantines and/or travel restrictions.
Genomic sequencing of as many cases as possible should be attempted for surveillance purposes. This allows individual cases to be attributed to outbreak clusters, with the high, but constant, rate of mutation of the virus being used to estimate the number of onward transmissions within each cluster at any given time. Then, the expected number of cases can be calculated and compared with the observed number to guide the extent to which further contact tracing should be performed.
While these actions are by themselves sufficient to prevent the majority of transmissions, they must be performed sooner rather than later, with the aim of stopping the spread of the virus throughout the community as soon as possible. Merely acting on the basis of test results is insufficient, as time is of the essence when dealing with exponential growth, and the picture painted by these test results is already a week or more out of date. Should they fail, mass lockdowns of entire cities and restrictions on daily life are then the only way to buy enough time for contact tracing efforts to work. Given the infectivity of SARS-CoV-2 and the insufficient number of beds, anything less will only delay the peak number of infections with no meaningful relief on the healthcare system while at the same time causing extensive disruption to a nation’s economy[18].
Will there ever be a vaccine?
It is true that numerous efforts are ongoing to develop a vaccine for SARS-CoV-2, which, if successful, will render the above precautions moot. However, they face the same problems faced by previous attempts to develop a vaccine for SARS. Creating a vaccine is inherently difficult, as it requires the selection of a vaccine target that is effective against stopping viral infection but which does not cause unwanted side-effects.
Similarly, the genetic diversity of coronaviruses creates the possibility that antibody-dependent enhancement might occur - that antibodies effective against one type of coronavirus would act as a Trojan horse that might even allow other, nonpathogenic human coronaviruses, or even a sufficiently mutated strain of the current virus, to efficiently infect cells, producing a worse outcome[19]. While difficult, these problems can be solved with sufficient time and effort, but to place hopes of containment on a rushed-out vaccine would be a dangerous and irresponsible action.
What can I do?
You need to play your part in protecting yourself from being infected by viruses in the environment.
It is important to recognise that SARS-CoV-2 is primarily transmitted by droplets, particularly of the sort produced by the very act of breathing or talking. These minuscule droplets are smaller than the width of a hair, and have been proposed to arise from the formation and rupture of thin layers of liquid in the throat and terminal bronchioles[20]. Droplets of this size can pass through a regular surgical mask, and are small enough to be suspended by air currents for hours[21]. This underlies the ability of this virus to infect people up to 5 meters away[22], and in rare cases, to even spread from house to house via incompletely sealed sewage systems[23]. Thus, complete protection will require a N95, or better, mask in conjunction with suitable eye protection such as a visor or goggles and other personal protective equipment, although even something as simple as a tea cloth or surgical mask will reduce your exposure to these droplets by 60-80%[24]. Even so, more prudent measures will suffice for those who are not on the front lines of dealing with the virus. These measures include basic precautions such as keeping a 2 meter distance when talking to others, wearing a mask especially if you are ill, and avoiding large groups of people.
 Another understated risk is the possibility that your hands might transfer viral particles (virions) present in the environment to your face. Despite being an enveloped virus, the virions are relatively stable when dry and have been shown to last for up to a week on a range of organic and inorganic surfaces kept at room temperature[25]. Thus, you should regularly disinfect any surface that is frequently touched, and you should also make a point of disinfecting your hands for a sufficient length of time before touching your face. Thankfully, being an enveloped virus, coronaviruses are fairly easy to inactivate. Any soap, detergent or any strong disinfectant such as 70% ethanol, 10% bleach or povidone iodine is enough to reduce infectivity by a factor of a thousand within the first 30 seconds of contact[25]. High temperatures and exposure to direct sunlight will also inactivate it, albeit over a much longer period of time[26].
Another understated risk is the possibility that your hands might transfer viral particles (virions) present in the environment to your face. Despite being an enveloped virus, the virions are relatively stable when dry and have been shown to last for up to a week on a range of organic and inorganic surfaces kept at room temperature[25]. Thus, you should regularly disinfect any surface that is frequently touched, and you should also make a point of disinfecting your hands for a sufficient length of time before touching your face. Thankfully, being an enveloped virus, coronaviruses are fairly easy to inactivate. Any soap, detergent or any strong disinfectant such as 70% ethanol, 10% bleach or povidone iodine is enough to reduce infectivity by a factor of a thousand within the first 30 seconds of contact[25]. High temperatures and exposure to direct sunlight will also inactivate it, albeit over a much longer period of time[26].You should also play your role in restricting the spread of SARS-CoV-2 in your own community. Defer or cancel any unnecessary travel and avoid gatherings of large groups of people in the short term, especially if you are unwell. If a quarantine order is announced, comply with it to avoid unnecessarily spreading the virus further. If you begin showing symptoms of the flu, self isolate as much as possible while waiting for medical advice, and stay away from high risk populations such as the elderly or infirm. It may be worthwhile to stock up with a few weeks of supplies in the event you do need to self-quarantine, but you should avoid panic buying excessive quantities of food or toiletries to prevent shortages which will only affect others and create the potential for wastage once they expire. While these actions may seem onerous on the face of it, they are necessary for the safety of yourself and those around you in the face of a pandemic.
Clifford Sia is a medical student at the University of Cambridge.
