TUESDAY, 26 MARCH 2024
Hypoxia is often considered as a harmful physiological diseased state. Physiologically, hypoxia is defined as a state with insufficient oxygen to maintain homeostasis. On a cellular level, depriving a cell of oxygen causes cell death. For a human, acute hypoxia (e.g. a stroke) can lead to irreversible damage to the brain and other tissues.Hypoxia is not always damaging. Regional hypoxia is common in our daily life. When exercising, the oxygen consumption of muscle tissue exceeds the rate of uptake from the blood. This causes regional hypoxia of the muscle, and the body will respond to maintain homeostasis. During exercise, metabolite (such as lactic acid) accumulation causes local vasodilation (dilation of blood vessels). Your heart will also beat faster to increase cardiac output. Together, this increases the flow rate of blood in the muscle. The ventilation rate at the lung will also increase to maintain the haemoglobin saturation of oxygen and remove excess carbon dioxide.
The response to hypoxia, being far from beneficial, is best considered a compromise in order to prevent damage. These procedures come with a cost. In order to allow for more blood flow to exercising muscles, arterioles of the digestive tract are constricted. MAP (which is normally highly controlled around a set point) increases slightly during exercise. This is an allostasis response: the host reaches a new equilibrium in response to stress factors. The allostasis response can not be maintained in the long term. As long as the host stops exercising, the body will return to the resting state.
Intermittent hypoxia is an alternation of normoxia (normal oxygen supply) and hypoxia. It is often related to obstructive sleep apnoea (OSA). OSA happens when the muscles at the back of the throat relax and block the airway during sleep. Being overweight is the main risk factor for OSA; excess fat in the neck increases the stretch of the muscle and is more likely to block the airway.
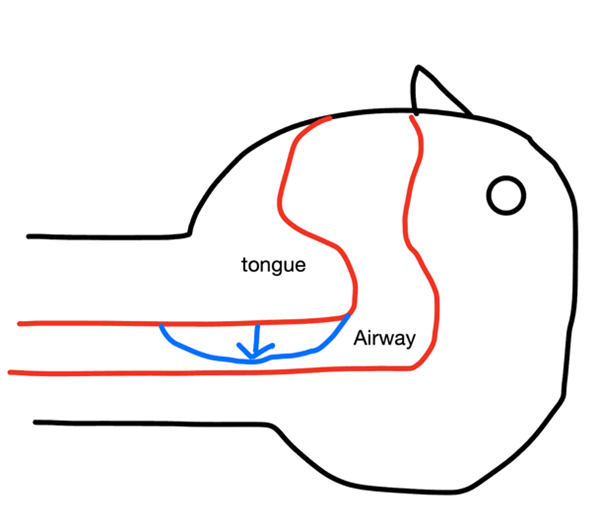
Fig.1 Obstructive sleep apnoea.
OSA does not cause much damage to the body, but it will cause significant interference in the life of the patient and their family. The vibration of a narrower airway produces loud snoring, which makes one’s roommate suffer. When the central chemical receptors detect increased pCO2 inside the cerebrospinal fluid due to hypoxia, the brain will force the patient to wake up and reopen the airway. This pattern can repeat more than ten times per hour. Although the awakening is not always conscious, patients with OSA often feel very tired during the day.
One can see that OSA is disastrous to a person’s (and probably his roommates’) life. However, increasing evidence shows that artificial intermittent hypoxia (IH) can be beneficial in the long term. Different from OSA, artificial IH is controlled and can be used to treat disease or improve health.
The most obvious benefit is increasing the rate of erythropoiesis (the production of red blood cells (RBCs)). We can compare people experiencing IH with people experiencing high-altitude hypoxia. At high altitudes, pO2 (the partial pressure of oxygen) inside the atmosphere is low. As a result, the haemoglobin will not be saturated, which reduces the oxygen-carrying capacity of the blood. Visitors from the sea level will compensate for this drop in pO2 by increasing the ventilation rate. However, in this case, hyperventilation will not help. pO2 inside the alveolar can never go beyond that in the atmosphere. Instead, this will cause respiratory alkalosis since too much CO2 is removed. CO2 dissolves in the blood and dissociates into HCO3- and protons. At a lower pCO2, the concentration of protons will be lower, resulting in a higher pH. The central chemical receptors detect increased pH in cerebrospinal fluid (CSF) and inhibit hyperventilation. There is another potential problem of generalised hypoxia. In local hypoxia inside the lung (e.g. the blockage of a single alveolus), the lung will shunt the blood flow to more appropriate areas by vasoconstrictions. But for generalised hypoxia in high altitude, too much vasoconstriction will increase the pressure in pulmonary capillaries, which causes oedema. The situation will be much different for local residents. Local residents adapt to the low pO2 by increasing erythropoiesis. Increasing the amount of RBCs (and thus haemoglobin) will increase the carrying capacity for oxygen. They can obtain enough oxygen even if atmospheric pO2 is low and prevent generalised hypoxia.
The challenge OSA patients face is similar to tourists at high altitudes. Because of a narrower airway, the ventilation rate of OSA patients decreases. The partial pressure of oxygen inside the alveolar will decrease, and the partial pressure of carbon dioxide will increase. The key difference here is that people at high altitudes are able to get rid of CO2 inside their bodies, but an OSA patient will gradually accumulate carbon dioxide inside the alveoli. Higher pCO2 will increase the ventilation rate or wake the patient up to open the airway. In artificial IH, unlike OSA patients, people can exchange CO2 with the atmosphere. The effect will be similar to that in high altitudes so that they can increase RBC concentration in the long term.
From an evolutionary perspective, animals are good at dealing with deficiency but find it hard to deal with excess. Obesity has become a serious problem in the population, and there are few intrinsic mechanisms to deal with it. Cells under hypoxia stress recruit a powerful transcription factor HIF. In controlled IH, we could utilise HIF to treat obesity. Humans can not respire fatty acids anaerobically, meaning that we can not consume fatty acids in hypoxia. This seems to contradict the previous statement: people with obesity have excess storage of fatty acids, and patients need to get rid of them. However, under IH conditions, HIF upregulates glutaminolysis (breaking down amino acids glutamine) to generate ATP and downregulates fatty acid synthesis to compensate for decreased fatty acid oxidation. In the long term, it is shown that HIF can increase the reliance of fatty acids for aerobic respiration. As a result, after a period of IH treatment, fatty acids are more likely to be respired and less likely to be produced, solving the problem of obesity.
Surprisingly, IH treatment can also improve immunity in inflammation. During inflammation, infiltration of leukocytes and activation of oxygen-consuming enzymes will cause local hypoxia. This hypoxia recruits HIFs, which then initiate the translation of a series of proinflammatory cytokines such as IL-1β and NF-κB. Together, these cytokines augment the immune response of the host.
It is possible that IH treatment can relieve stress-related disorders. The hypothalamic-pituitary-adrenal (HPA) axis controls the release of glucocorticoids, such as the stress hormone cortisol. The HPA axis is normally regulated by negative feedback mechanisms. However, stress-related disorders and depressive disorders are often caused by dysregulation of the HPA axis. Hypoxia will activate the HPA axis in a dose-dependent manner. Prolonged hypoxia can induce stress response and the release of stress-related glucocorticoids from the HPA axis. In controlled IH, to reach a new set point of stress hormone level, adaptation of the HPA axis will increase the power of negative feedback. When the stress factor (hypoxia) is removed, this stronger negative feedback will be used against stress disorders.
Finally, we can imagine IH treatment as a vaccine. We are stressed in a controlled manner that is not severe enough to cause damage. If a patient can adapt to this external stress, he can improve his performance in future encounters. However, the time and pattern of IH treatment is critically important. Maladaptation can have detrimental effects on the patient. There is still a long way to go for applying IH clinically. In the future, it would be a potent way to treat disease by utilising mechanisms inside our bodies.
Article and diagram by Mingshuai Zhu.
Image credit: Pixabay, released under the license Creative Commons Zero (see here).
